Obesity: Is it in our genes?
Obesity-related health issues are on the rise. Data released by the Australian Government last year showed 60% of men and 66% of women had a waist circumference putting them at high risk of health issues.
Type 2 diabetes, cognitive impairment, stroke and heart disease are no longer relegated to being health concerns for seniors.
In understanding obesity, there is a big question troubling researchers and health professionals: could genetics be playing a role in the global obesity epidemic?
The answer is complicated.
We still have a lot to learn about the genetics of obesity, but research is suggesting our genes are not our destiny.
It is the interplay of environment, behaviour and genetics driving the obesity health crisis in Australia and around the world.
Obesity and genetics
Obesity resulting from monogenic (single-gene) mutations have been known about for some time.
These mutations normally occur in genes affecting appetite control, leptin (fat) metabolization and melanocortins, the small group of hormones active in regulating food intake.
However monogenetic mutations are rare and often linked to other health issues.
Common obesity in DNA
What we call “common obesity”, the condition affecting almost one-third of Australian adults, is a different story.
Researchers are looking for answers by scanning thousands of complete DNA sets to find the gene variations that could play a role in obesity.
There may be hundreds of genes linked to common obesity. Slight variants in the DNA strands containing these genes can change their behaviour, which in turn impacts:
- Skewed energy balance
- Reduced energy expenditure
- Abnormalities in fat storage
- Increased feeding behaviour
A 2007 study confirmed the first gene variant affecting BMI. The thousands of Aussies potentially carrying this variant are up to 30% more likely to face obesity.
To date, more than 30 potential gene candidates on 12 chromosomes associated with BMI have been identified as targets, although more time is needed for conclusive studies.
However, the genes themselves may have only a small impact on weight gain.
In fact, a 2008 study proved the variant identified in the previously mentioned study could be offset with physical activity.
Therefore, gene variants are highly unlikely to be the lone culprit in rising obesity rates.
Genetic-environment interplay
Most people are likely to have some genetic predisposition to obesity from birth.
Experts in the field are clear on one key thing: genetics play a significant role in an individual’s susceptibility to the “obesogenic environment”.
That is, the combination of environment and physiology that leads to being overweight.
These genetic handicaps prejudice people to increased high-calorie food intake and low levels of physical activity by affecting appetite and energy levels.
But there is good news: the (relatively new) field of genetic-environment relationships suggests there are several things adults, children and seniors can do to reduce their risk of obesity:
- Increase physical activity
- Reduce sedentary activities (watching TV, using computers)
- Limit the availability of unhealthy food
- Investigate weight loss surgery options
These solutions may seem like common sense but when paired with cutting-edge genetic research, a pattern of behaviour to combat obesity begins to emerge.
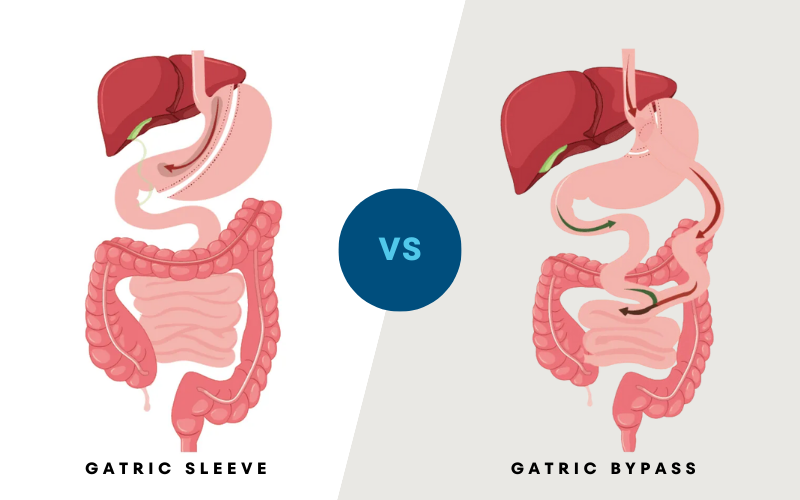
Weight loss options
Aging increases the severity of obesity-related health risks, but obese and morbidly obese adults are facing an uphill battle against a combination of genetics and lifestyle.
For obese and morbidly obese Australians, bariatric surgery is an effective tool to lose excess weight and enable a healthier environment.
Contact Perth Weight Loss and Surgery to understand if you qualify for weight loss surgery.